PeekMed
Communication is essential in the operating room – and even in the pre-procedure moment, before entering the Operating Room. Bad interaction between all parties might lead to several types of complications – such as being one of the causes of wrong-site surgery.
To prevent this type of situation, we've prepared a short 5-step guide to help you prevent wrong-site surgery:
Apart from the 5 steps (or strategies, if you prefer), we also prepared a short definition of what is a wrong-site surgery and a resume on why it might not be fully implemented yet.
What is Wrong-site Surgery?
Wrong-site surgery is a generic term that includes a moment where an adverse event leads to preventable errors. Wrong-site surgery includes the wrong procedure, wrong patient, wrong side, and wrong surgery site. Most of these mistakes are generally caused by a lack of a formal system to verify the site of the surgery or a breakdown of the system that verifies it.
Simple strategies are implemented before procedures are performed to prevent wrong-site surgery – reducing drastically clinical, logistical, and medical errors. And if you do not know which ones are the better, fear not.

1. Pre-procedure Verifications: Do you have everything you need?
Missing information or materials might be the first problem in a surgical team agenda. This happens before even entering the Operating Room.
To prevent this, you should consult all the information related to the patient. From labeled diagnostic analysis to radiology exams or images, it might be a problem if you enter the OR without information that might support or validate the procedure you are doing.
The same happens with required items. This includes blood, special equipment, and devices. In the case of orthopedic surgeries, ensuring that you have the best-suited implants is also essential.
Realizing you can’t do the procedure because you are missing the correct implant (or most suitable size) might be a dramatic situation for your patient. This is why preoperative planning is so important.
2. Surgical checklist: are you ready?
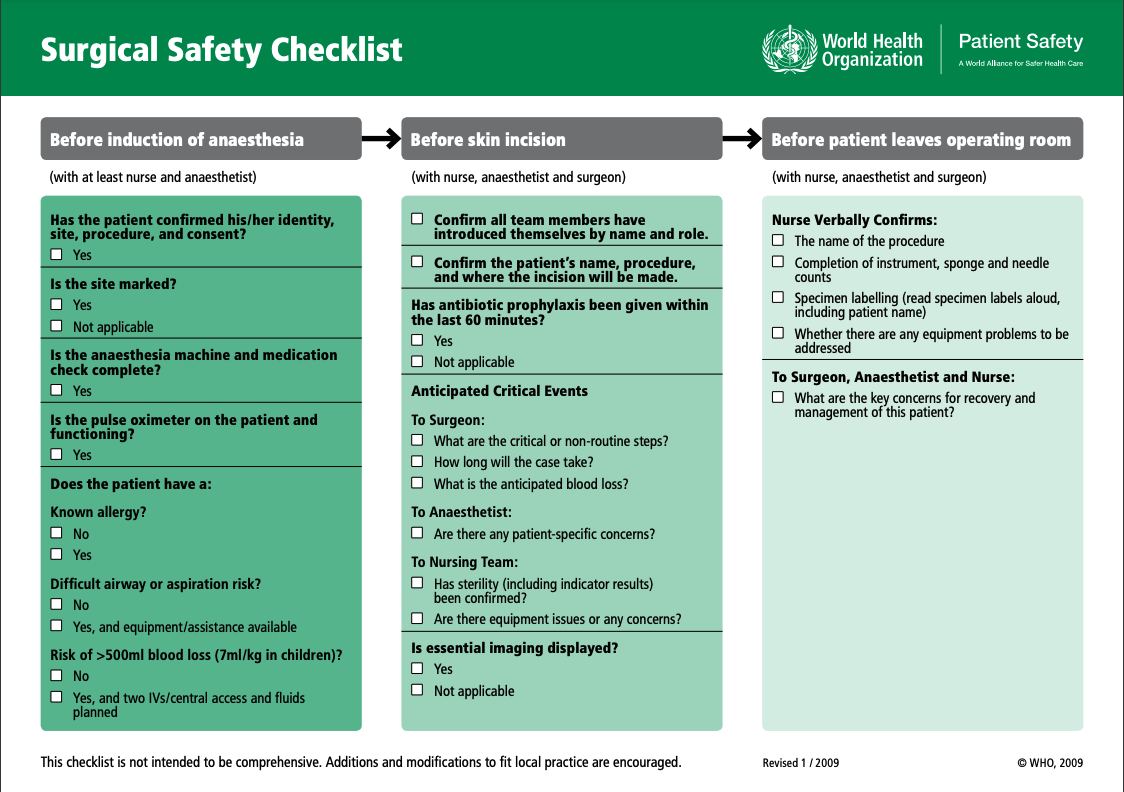
Studies show that implementing surgical safety checklists is an effective way to improve patient safety by decreasing both complications and mortality.
But are you wondering: what is the intention of a universal protocol? It means to prevent a human error – preventing wrong-site procedure situations
The use of a checklist identifies everything that needs to be done preoperatively, including marking the side and site of the surgery. Often, hospitals choose to have a checklist displayed within the OR – previously on a poster, and nowadays on the monitor strategically positioned, so that every provider can watch the circulating nurse check off the essential steps.
A starting point might be the World Health Organization (WHO) checklist. Taking specialist consensus, this safe surgery checklist focuses on four main areas: surgical site infection prevention, safe anesthesia, safe surgical teams, and measurement of surgical services.
Following the same idea, the Joint Commission developed the Universal Protocol Surgical Checklist which is also focused on preventing wrong-person surgery and related incidents by introducing a checklist – or protocol, if you prefer.
This protocol was implemented in 2004, following a significant report of wrong-site surgery issues.
To develop this Universal Protocol the Joint Commission collected expert consensus on principles and steps to prevent wrong-site, wrong-procedure, and wrong-person surgery.
This consensus led to the implementation of the Universal Protocol in Hospitals and medical centers, mandatory for accredited institutions.
3. Site Marking: prevent surgery to be performed on the wrong limb
A leg marked with capital letters saying “NOT THIS LEG” is an iconic moment of medicine that even became a meme on TV shows. While it might seem like a joke, this is a real procedure suggested by several institutions, like the Joint Commission.
What has been suggested is that, when there is more than one possible operative site or location for the procedure, measures should be taken to ensure that no one involved in the process is sure and constantly reminded of what we are doing.
While this is extremely important for limb surgery – where you want to make sure you are performing the procedure on the right or left leg – it’s not the only case where it applies. In spinal procedures, for instance, it’s important to mark the general spinal region on the skin.
4. Surgical time-out: the last step
Performing a surgery “time-out” is the last step before starting a surgical procedure. The Joint Commission (JCI) recommends that the procedure is not started until all questions and concerns are resolved.
But how to perform a time-out?
A designated member of the team starts the time-out for all the team members involved in the procedure – from physicians to nurses, and the operating room technicians. At this moment, all members communicate actively.
During the time-out, the team agrees on:
- Who is the patient they are operating on;
- Correct surgery site where the procedure is being done;
- Which procedure to be done;
This communication moment can include the patient too:
5. Talk to the patient to prevent errors in the surgery
While validation from official documents is very important, the patient may be a keystone in the process, too.
Simple interactions with the patient help prevent great mistakes. Questions that you might ask the patient to prevent wrong surgery, wrong person, and wrong-site issues:
Your name is Mr. Jones, right?
Mr. Jones, we are operating on your right knee today. That’s correct?
Can you point at your right knee?
We will be performing

Wrong-site surgery: can we prevent it?
Yes, we can prevent wrong-site surgery issues. For that, checklists and protocol implementations, those elaborated by the World Health Organization (WHO) and the Joint Commission’s Universal Protocol, are extremely useful.
However, some healthcare professionals might be resistant or hesitant to implement them, because they feel immune to errors or that it might be a waste of time.
Wrong-site surgery still happens 40 times a week in the United States. Data from the American Academy of Orthopedic Surgeons (AAOS), suggest that in the case of an orthopedic surgery, it has a 25% chance of happening.