PeekMed
Knee pain is a common complaint for many patients and it’s often related to the overloaded compartment of the knee due to metaphyseal bone deformity of the tibia or the femur.
This leads to the knees becoming deformed, either by becoming significantly apart when standing – varus knees – or for them to touch each other when the patient is standing – valgus knees.
To address this, orthopedic surgeons perform knee osteotomy procedures. The procedure can be used to correct an abnormal size, shape, position, or composition of the leg.
High tibial osteotomy (HTO) surgery is used for varus deformities and distal femoral osteotomy (DFO) is for valgus deformities. These are also known as varus knee valgus osteotomy and valgus knee osteotomy, respectively.
Overall, both knee tibial osteotomy and femoral osteotomy of the knee might be necessary to plan leg alignment before the surgical procedure – a knee realignment surgery.
When planning how to perform knee osteotomy, surgeons might conclude that, in complex cases, a single-level osteotomy will not adequately address the deformity.
Thus, it might be necessary to perform a combination of both osteotomies around the knee to perform leg alignment. This is often referred to as double-level osteotomy (DLO), Total Knee Osteotomy (TKO), or double osteotomy of the knee.
Putting it simply, a combination of DFO and HTO knee surgery.
This technique allows surgeons to realign the bones on either side of the knee joint. While some might think that this complex procedure might not be worth the risks, the truth is that technology does make it much more manageable.
Below, we will be exploring how. Remember that regardless of whether it is a simple osteotomy or a complex one such as the one we will be presenting, a preoperative planning tool allows orthopedic surgeons to gather all the information in a matter of seconds.
Case study on how to perform a double knee osteotomy
A 61-year-old man, non-smoker nor diabetic, with a previous proximal tibial trauma, presents crippling medial knee pain.
This made him incapable of walking for more than 100 meters and had knee varus deformity but preserved his range of motion.
After the x-ray is analyzed, the orthopedic surgeon thinks about a knee-high tibial osteotomy.
However, he asks a colleague for a second opinion, as he is not familiar with such big deformities. The main concern is that the high tibial osteotomy for varus knee opening may be exaggerated.
After confirming that knee osteotomy surgery was necessary, surgeons started to plan an osteotomy of the knee surgery.
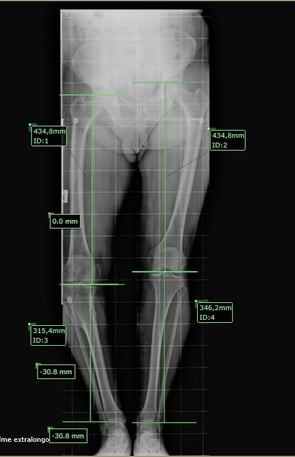
Using PeekMed, surgeons gained quick specific insights regarding the patient-specific body.
It was noted that the patient has a metaphyseal deformity of both the tibia and the femur.
In this scenario, PeekMed’s knee osteotomy planning tool allows surgeons to automatically and successfully identify both deformities.
Hence, using artificial intelligence, PeekMed suggested a double-level osteotomy instead of the high-tibial osteotomy surgery that was initially proposed.
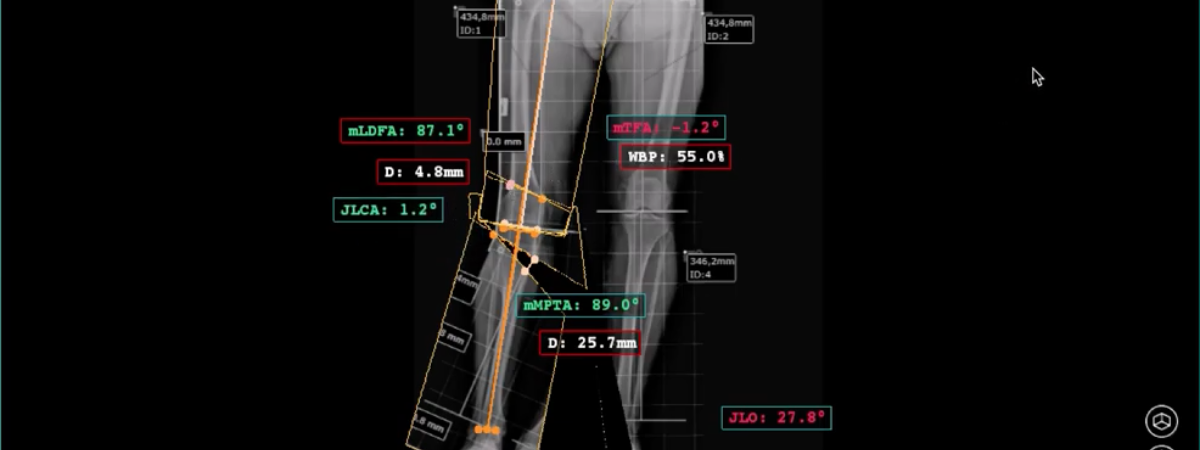
As can be seen in the image and the video, surgeons gained quick, automated insights regarding all the possibilities and necessary angles to perform the preoperative planning.
After carefully planning all possible outcomes, the patient underwent the planned double-level osteotomy – which included both high tibia osteotomy and distal femoral osteotomy.
The patient obtained a positive functional result, keeping the range of motion, and improving gait and pain at 6 months postoperatively.

|

|

|